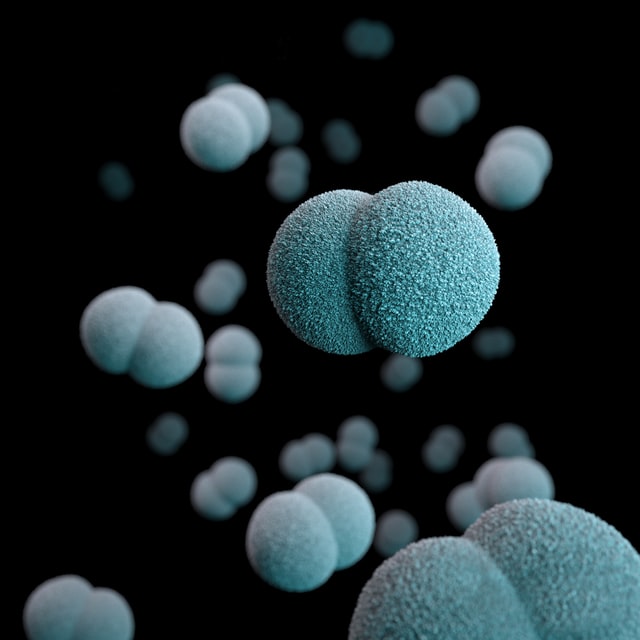
Oral Bacteria leads to serious respiratory issues
Oral biofilms, periodontitis, and pulmonary infections
Bacteria from the oral biofilms may be aspirated into the respiratory tract to influence the initiation and progression of systemic infectious conditions such as pneumonia. Oral bacteria, poor oral hygiene, and periodontitis seem to influence the incidence of pulmonary infections, especially nosocomial pneumonia episodes in high-risk subjects. Improved oral hygiene has been shown to reduce the occurrence of nosocomial pneumonia, both in mechanically-ventilated hospital patients and non-ventilated nursing home residents. It appears that oral colonization by potential respiratory pathogens, possibly fostered by periodontitis, and possibly by bacteria specific to the oral cavity or to periodontal diseases contribute to pulmonary infections. Thus, oral hygiene will assume an even more important role in the care of high-risk subjects – patients in the hospital intensive care and the elderly. The present paper critically reviews the recent literature on the effect of oral biofilms and periodontitis on pneumonia.
Pneumonia is an infection of the lungs caused by bacteria, mycoplasma, viruses, fungi, or parasites. Bacterial pneumonia is a common and significant cause of mortality and morbidity in human populations. Pneumonia together with influenza is a top ten cause of death in the world, and in elderly nursing home residents the leading cause of death. Pneumonia also results in morbidity and considerable decline in the individual quality of life as well as in increased medical care costs for the healthcare system. Bacterial pneumonia includes community-acquired pneumonia and hospital-acquired (nosocomial) pneumonia. Nosocomial pneumonia, occurring >48–72 h after admission to a hospital or nursing home, can be divided into two subtypes: ventilator-associated pneumonia (VAP) and non-VAP. Pneumonia accounts for 10% of infections in intensive care units (ICU) being the most common infection in this hospital setting (Vincent et al, 1995). The onset of pneumonia can easily double the length of the patient’s hospital stay, and the cost of VAP treatment has been estimated to average as high as $40 000 per patient (Rello et al, 2002). Pneumonia is also prevalent in nursing homes, comprising 13–48% of all infections (Crossley and Thurn, 1989). The mortality rate of nosocomial pneumonia can be as high as 25%.